Our March 2024 LMCC meeting took place on Wednesday, March 27 at 5:30pm via Zoom. (Because of the expected storm and 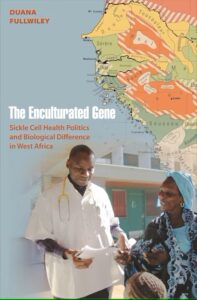 because Thursday was a campus Well-Being Day, we opted to hold this meeting exclusively via Zoom. For our April meeting, we plan to meet once again in UNC’s HHIVE Lab, Greenlaw 524, with a Zoom option as well.)
because Thursday was a campus Well-Being Day, we opted to hold this meeting exclusively via Zoom. For our April meeting, we plan to meet once again in UNC’s HHIVE Lab, Greenlaw 524, with a Zoom option as well.)
For our March meeting, we discussed The Enculturated Gene: Sickle Cell Health Politics and Biological Difference in West Africa by Duana Fullwiley (Princeton UP, 2012). Specifically, we discussed:
- Preface (pp. ix-xxiii)
- Chapter 2: “Healthy Sicklers with ‘Mild’ Disease: Local Illness Affects and Population-Level Effects” (pp. 45-76)
- Optional/suggested reading: Chapter 1: “Introduction: The Powers of Association” (pp. 1-44)
If you missed the meeting, you can still access the text on the Readings page of this site!
You can also access the recording of our meeting here.
Our next meeting (and our final meeting of the semester) will take place on Wednesday, April 24 at 5:30pm in UNC’s HHIVE Lab, Greenlaw 524. If you can’t attend in person, you can attend in real-time via our usual Zoom link. We will send out an announcement soon with more information for that meeting.
A few reminders and announcements:
- Be sure to follow LMCC on Twitter and Instagram to show your support and receive regular updates!
- If you want to get more involved with LMCC, please send us other resources we should post to the site or suggestions for improvements, additions, future readings, etc. We’d love to hear your ideas and input! (See our email addresses on the Home page of this site.)
- Also, please feel free to spread the word about LMCC to other interested graduate or professional students at UNC.
Fullwiley, Duana. The Enculturated Gene: Sickle Cell Health Politics and Biological Difference in West Africa. Princeton UP, 2012. https://www-degruyter-com.libproxy.lib.unc.edu/document/doi/10.1515/9781400840410/html#contents.
Some key concepts:
- This particular reading is a productive shift away from recent Euroentric readings
- Fullwiley’s book challenges the way in which biomedicine (in this case, genetics) is prioritized as the empirical, objective truth (at the population level, ignoring individual realities)
- Discourse around sickle cell, process through which it was defined as “mild” in Senegal/challenging rhetoric of genetics as the truth
- Ethics of narrative, and structure of discovery: what were things like before putting a name to sickle cell, larger social history
- The historical context of sickle cell anemia, often taught from an exclusively medical/biological perspective
- Sickle cell disease continues to be obscured, perceived as mild, forcing individuals to take agency for themselves
- According to the date, 1 in 10 Senegalese are affected by sickle cell (as of the book’s publication, 2012); 10% of the population has to live with some form of this condition. This must surely create a significant impact on caretakers and family and friends; discourse about it being “mild” as being somewhat commonplace and thus how it may become normalized
- Individuals interviewed in the chapter are not dismissive of the condition, but often consider it as part of an identity/of how to live with it
- Social responsibility to take care of “sicklers” (Fullwiley’s term for people with sickle cell disease)
- The metrics of “mildness” and priority and occurrence and necessity all involved in the terming of a condition as “mild”
- Implication regarding marriage and relationships; the cultural imperative to reproduce; a sickler being potentially shunned by a support community for marrying another sickler
- The biological determinism around two sicklers marrying and procreating leading to a child who also has sickle cell disease (socially discouraged to avoid producing such a child)
- Similar conversations take place about people who have autosomal dominant conditions (like certain forms of dwarfism or Huntington’s disease) having children as well
- Why one sickler might desire another sickler as a romantic partner: shared community and mutual understanding of one’s situation; potential grace/understanding from mothers-in-law and other members of the partner’s family
- Economies of kinship as a resource for support and survival
- What does someone with sickle cell disease look like? How do you give space to someone to talk about how much the disease sucks?
- Notions of an “invisible disease” or one that only appear/become legible periodically, via waves or moments of “crisis”
- All bodies anticipate illness; all bodies will eventually experience illness/disability
- Countries, advocacy organizations, and even individuals come to “compete” with each other for international attention and NGO support/awareness/funding
- Potential tension between interviewer’s perceptions of the interviewee’s health and his own perception of his health
- Different moments of travel: the DNA passport, crossing the Atlantic, transatlantic slave trade, crossing paths of cultural spaces; work of building a model of understanding a complex network that allows these narratives to emerge and systems to take the form they have now; we want to be mindful of all who are implicated in this system, while still maintaining fidelity to the sickness; it’s not enough to take for granted those living with the illness without the resources needed to feel better
- What happens when there’s a lack of infrastructure and resources; just because people with a particular illness or disease can adapt doesn’t mean they should have to, nor does it get anyone (governments and other civil support systems) “off the hook”
- The FDA just approved (within the past few weeks, 2024) the first CRISPR to address sickle cell disease; it’s a complete cure, but an arduous and wildly expensive tool that will not be accessible to anyone in Senegal; kind of a dark cloud over the reading; Vox has a video on the approval and the process; see also https://www.scientificamerican.com/article/fda-approves-first-crispr-gene-editing-treatment-for-sickle-cell-disease/
- Even in terms of kinship and the rhetoric of “sharing blood” not as biological family but as people sharing blood via the same condition, one’s condition could be interpreted as part of one’s identity; the treatment literally kills off the condition in one’s body, and this is potentially threatening to one’s sense of identity
- There are dimension to add to the text: kinds of non-Western interventions and how that interacts with new technologies
- The CRISPR procedure will involved various levels of access via socioeconomic status, patient viability (not having other pre-existing health concerns); different organizations or groups competing for funding; individuals competing to be included in this list as viable candidates for trials and then for this procedure more widely. There is a kind of performativity to be “a viable candidate.”
- NGOs (and other similar organizations and entities) may be well-intentioned, but they are not just promoting Western approaches to medicine; they often come with a lot of other political and social imperatives.
- There is no singular disease ontology; instead there are multitudes of ontologies for any disease or condition, especially in the case of sickle cell disease
- Western scholarship and medicine emphasizes the value of “empirical/objective truth,” but Fullwiley problematizes this rhetoric that prioritizes empirical/quantitative truth and instead emphasizes “relative affectedness” for any condition, especially (in this case) sickle cell disease.
- The categorization of diseases will create differences, but categories can also create unities, creating a community that works together
- Consider the notion of “triage” in the medical humanities (and thus a set of priorities); how to determine what is a priority; how scientific advancements are developing and using a language that moves into systems of normalcy versus weaponization; might the Senegalese government think they have some control over the disease? What are the metrics of priority?
- Where is the support going to be the most effective (who needs it most vs. positive outcomes)? Different levels of support/priority might be in conflict among these various levels of potential support (individual, community, national, and international)
- How many individual severe cases have to emerge before these severe cases are no longer perceived as “outliers” and the disease is considered serious rather than “mild”?
- The performativity of illness is always a double-edged sword; what is the severity of that disease in the neighbor? Maybe there is a medical actuality to the mildness, coupled with the desire for mildness. A desire to perform normalcy because they were locked out of social opportunities can sort of clash between medical actuality, a person’s own performativity of disease, and other’s perception of the person
Some key passages:
Preface (pp. ix-xxiii)
“This book is a medical anthropologist’s attempt to document how people enact what it means to have sickle cell anemia, a familiar enough condition, in a place less well known, Dakar, Senegal. In it I argue that patients with sickle cell express the symptoms of this blood disease through their bodies and biology, yet they do so by articulating pain, health, and normalcy in light of idioms of kinship, colonial histories of race, postcolonial population genetics, material medical lack, and failed health infrastructures that mark nearly every aspect of their lives. Ultimately I claim that sickle cell, like any disorder, has no singular disease ontology that could possibly be stripped from the historical and political structures in which people affected live. Social actors—patients and families, as well as scientists, doctors, and healers—have brought about specific experiences of this disorder in their everyday struggles with the economics of health care, in their efforts to reorder their global standing, in their hopes to establish scientific authority, and in the survival tactics they forge through therapeutic social supports with others. Together they conjure sickle cell well- being in the face of systematic health triaging in the global South” (Fullwiley ix).
“I focus on how people embody sickle cell variation and differential lived expressions of sickling blood through historical, personal, scientific, and political processes that yield forms of life where biology and cultural strategies for living well are perpetually interlocked” (Fullwiley ix).
“…sickle cell science could never be neutral or devoid of judgments about human similarity and difference” (Fullwiley x).
“…sickle hemoglobin became an all-too-reliable weather vane for the climate of race thinking in the United States, as many physicians had long obsessed over black versus white biological differences” (Fullwiley x).
“This idea of relative affectedness, in different configurations, would remain central to later scientific narratives of Senegalese sickle cell particularity. It is at these points of conceptual departure where we begin to trace the health politics of sickle cell biological difference in Senegal today” (Fullwiley xi).
“…it was a potential metric to size and order ethnic differences on the ground. With [Léon] Pales leading several studies, the French followed British surveys conducted in East Africa in the late 1940s in their assumption that one would find different rates of sickle hemoglobin in the blood of ethnic groups defined and classed by language, cultural forms, and, in some cases, homelands” (Fullwiley xi).
“…key colonial physician-anthropologists, such as Pales, stressed how ostensibly different and multiple groups of black Africans varyingly exhibited this so-called African pathology across the geopolitical terrain of French West Africa…. The pattern of that variation, it was assumed, would congeal ethnicity and race into a metonymic configuration where mental telescoping would allow researchers to scan the geography of race for ethnicity within it” (Fullwiley xii).
“The area of Senegal was literally mapped as a geopolitical ethnic tableau of what the French administrators in question called biologie comparative for a range of traits, both morphological and serological” (Fullwiley xii).
“I want to stress here that the raw scientific emphasis on the differential penetrance of sickle cell anemia, again, the relative affectedness of the disease in different groups of Africans broadly, set the stage for future scientific thinking about sickle cell anemia as a phenomenon that could distinguish populations of black peoples, one from the other, across different African geographies” (Fullwiley xii).
“As we will see further on, today French geneticists and Senegalese sickle cell specialists continue to borrow from imagined ideas of African geopolitical identities, albeit now drawn along contemporary nation-state boundary lines, to explain sickle cell biological difference in West Africa” (Fullwiley xii).
“Today postcolonial economic asymmetries and ‘priorities’ set by global health agendas that have overlooked sickle cell anemia have actually helped bring into being a highly localized version of sickle cell on Senegalese soil. In part because sickle cell anemia was deemed an exotic pathology, rather than as a disease per se, during the period of ‘raciologie’ studies in colonial Senegal, specialty medical clinics and general medical education on its effects lagged” (Fullwiley xii-xiii).
“As we will see in the pages ahead, patients and scientific professionals symbiotically feed each other’s conceptions of sickle cell gravity or, more often in this case, functional sickle cell mildness” (Fullwiley xiii).
“In these everyday efforts many sicklers end up vindicating their doctors’ ideas that limited medical treatments in this setting, luckily, may work after all. I argue that it misses the point to try to freeze the frames of this moving tautology in order to discern which aspects of this dynamic necessarily animate the others. Patients’ survival tactics, such as their reliance on widespread botanicals, or, their participation in patient advocacy groups formed through biosocial blood ties that both mimic and renew idioms of kinship solidarity, create a perception that many instances of sickle cell are ‘managed,’ cared for, and less clinically urgent” (Fullfiley xiii).
“What is clear is that sickle cell anemia on Senegalese ground today has been lauded on multiple registers as an instance of relative African vitality, rather than solely as a prevailing pathology. Yet, as this book unfolds, it will become apparent that this disease conception—what I call a lived construct of mild Senegalese sickle cell anemia—should not be uncritically understood as a simple celebration of Afro-optimism. Postcolonial optics of Senegalese particularity, genetic technologies used to explain phenotypic differences, colonial legacies of racial science that obscured an emphasis on sickle cell as an actual disease, as well as the educational and medical lag that followed sickle hemoglobin’s racialized conceptions, have forced people to improvise survival strategies in the face of spotty sickle cell care in the present. Today economic precarity and what patient activists refer to as continued ‘state incomprehension’ and ‘neglect’ of their disorder add to the social and historical genealogies that spawn the recuperative disease ontology of ‘mild sickle cell anemia’ in Senegalese bodies” (Fulwiley xiv).
“In the United States, one need not look very far to see how haplotype markers, as biological tools of social and personal meaning, have become thoroughly intertwined with psychological needs and political conceptions of identity linked to African geography. They are sociotechnological products—never just about biology—that permit people to pack into truncated DNA code what might also be longer experiential life and historical processes of belonging that far exceed genetics alone” (Fullwiley xv).
“…in the French and Senegalese postcolonial setting of contemporary Dakar, sickle cell haplotypes have been used for over a quarter of a century to fill in specific voids in medical knowledge. In particular, African sickle cell haplotypes have been utilized to theorize a pathway of genetic causation that yields different biological outcomes with regard to how people manifest sickle cell disease in the clinic and beyond” (Fullwiley xvi).
“The marketability of this idea—the association between Senegalese sickle cell and better health—has, in its own way, spawned a genetic exceptionalism that now favors the Senegalese by pegging their sickle cell health to a biogenetic cause. Through their specific genetic markers, the Senegalese people are said to exhibit an especially mild form of sickle cell anemia whereby they do not become as sick as others who have the disease in Africa and its diaspora” (Fullwiley xvii).
“In this book I argue that with the HbS haplotype discourse, key French and Senegalese geneticists, hematologists, and pediatricians have made sickle cell genetic sequence variations correspond to a level of observed health in African bodies—bodies that are imagined to be nominally, and nationally, distinct. Following from this, I argue that the very epistemological categories of ‘Senegalese HbS,’ and the ontological lived disease that corresponds to it, obtain their descriptive powers through social dynamics of identity and difference rather than through any ‘natural’ means entirely free of such political machinations” (Fullwiley xvii-xviii).
“Ideas of difference that cohere through people’s imaginaries about belonging are often marked by place and nation. What this book describes on this front for people with sickle cell in Senegal has often been imposed from the outside but blended with social dynamics of survival within. The postcolonial relationship between France and Senegal continues to inform local medical science as well as economically inflect the illness it aims to treat, in emergent ways” (Fulllwiley xviii).
“New studies regarding sickle cell often focus on variations in people’s levels of fetal hemoglobin as well as the frequency at which they suffer sickle cell pain crises. I argue here, however, that these effects in the body should also be considered beyond mere population genetic framings. This is not to deny that biogenetic differences exist. To the contrary, we cannot but recognize that more of them are being discovered by the day, as genetic technologies push on. Instead, I ask, how is it that genetic explanations are allowed to absorb more complex social, medical, and economic processes in instances when observed health outcomes are correlated with genetic patterns, often despite any clear detailed proof establishing causation? What might happen to the seductive allure of genetic ‘association studies’ (where DNA is correlated with a given outcome) if an analysis of sickle cell biological difference in West Africa took seriously the concerted efforts and cultural practices that sickle cell patients themselves have put into surviving in the face of economic scarcity, limited treatment options, and intersubjective structures of care networks that allow them to aspire for health?” (Fullwiley xviii).
“Based on ethnographic research I conducted in Senegalese public university hospitals, traditional healing sites, French clinics and laboratories, Dakar market places, and patients’ homes over the course of more than a decade, I found that people’s ability to make-do with scant biomedical palliatives functionally filled a resource gap in which the state has proved incapable of adequately providing basic health care for most of its citizens. People’s ability to improvise self-care with therapeutic autochthonous plants (one of which has been hypothesized to also increase fetal hemoglobin), sometimes coupled with their investment in the numinous powers of their Islamic faith, or at least their faith in the therapeutic value of their social supports forged with caring others, were key factors that shaped their embodiments of this disease. When these actions combined to mitigate symptoms, the result could be reframed as Senegalese sicklers’ ‘positive health outcomes’ when seen from a biomedical perspective. Therefore disease embodiment and favorable sickle cell health have been mutually brought into relief as people have found ways to minimize the gravity of their situations” (Fullwiley xviii).
“These pressures, however stressful, were also aspirations that made people not only claim to ‘live well’ with sickle cell anemia but to live well despite it. This latter triumphant attitude was both an enunciation of the health they hoped to muster and a denunciation of the long state silence, public health invisibility, and general scarcity of medical resources that many patients faced when they were not feeling quite so well, and when they were more generally seriously afflicted with the deep malaise of another aspect of the future: economic uncertainty and ‘crisis’” (Fullwiley xix).
“Senegalese medical professionals have taken such stances only after sifting the data on biological difference through the sieve of a local health politics of scarcity. By this I mean that they became accustomed to comparing sickle cell with other global-local health priorities that command donors’ attention and thus dictate which diseases merit public visibility, ‘awareness,’ and subsidies for care” (Fullwiley xix).
“In this way ‘mild’ sickle cell anemia is, in part, a lived construct of economic triaging and uneven investment throughout Africa, where, as James Ferguson has argued, the ‘global,’ in this case global health, does not ‘flow,’ but rather ‘hops’ to connect privileged points ‘while excluding with (equal efficiency) the spaces’ and, I would add, health issues, that have not been ‘connected’ to Western aid interests and funding lines (Ferguson, 2006, 47). All throughout Africa we are witnessing a simultaneous dearth and excess of funds for health problems and their scientific solutions. In this blotchy matrix some diseases benefit greatly and others remain ignored” (Fullwiley xix-xx).
“I do not want to say that ‘severe’ cases of sickle cell in Senegal have never existed. Indeed they have. My strategy in the major part of this book, however, has been to follow instances of how the disease has been varyingly lived as mild, or how stoic subjective expressions of illness—as well as physicians’ belief that they are ‘blessed’ with treating a disease ‘type’ that may not require the importation of frontline therapies from the North—both permit and are permitted by the generative, and economically inflected, discourse of Senegalese sickle cell specificity” (Fullwiley xx).
“My purpose in writing this book has been to bring crucial concerns of cultural and medical anthropology to renditions of genetic science. In detail this means showing how both patients’ and medical professionals’ economic, health, and political struggles actively shape lived expressions of sickle cell biological difference in Dakar” (Fullwiley xx-xxi).
“Together histories, politics, and bodies, as biocultural products, must be brought into the increasingly pervasive technical story of haplotypes and population health for sickle cell, as the ‘first’ genetic disease, but also for countless other conditions that now figure in the annals of science. My goal here is to make human history and social practices bear on and, more importantly, to bear out our understanding of genetic data points. In an age when many facets of human life are gaining new senses as biologically destined through the precision of genetics, I chronicle the lives of Senegalese sicklers and document how the state of health care in the global South, international health priorities, colonialism, kinship, and histories of race all mark aspects of how Senegalese sickle cell has come to be associated with a modified clinical picture and favorable biological life course. Biology is not destiny. Nor, as Sociologist Nikolas Rose would have it, is it simply ‘opportunity.’ For many in the global South, postcolonial legacies, economic constraints, and struggles to define health options—despite the odds—clearly shape the kinds of chances, prospects, or breaks from genetic destiny people are able to make in the first place” (Fullwiley xxi).
“This is the first book to ethnographically treat a genetic disease in Africa. Not surprisingly the social scientific study of genetics has usually focused on richer locales, where technologies of diagnosis, as well as lay and medical education about them, are more pervasive” (Fullwiley xxi).
“As with most studies on scientific trajectories of illness, my ethnographic engagement with sickle cell in Senegal provides an aperture onto the societal forces that condition disease embodiment, but that also highlight the possibilities for how power shapes people’s subjectivities across the North-South divide. Sickle cell is one window through which we might better understand Senegal’s place in the world, its history of special status in the French colonial era, its population’s ability to cope with the difficulties of structural adjustment, and, in the postcolonial present, its economic dependency on multilateral institutions, as well as the ways this dependency affects which diseases it is able to prioritize, and which it is forced to neglect” (Fullwiley xxii).
“When the Senegalese government entered into economic structural adjustment in 1979, it was forced to drastically cut health-sector spending. In this context of scarcity, the discovery of sickle cell DNA haplotypes, and the attendant observation that the Senegal type was associated with a better health outcome on the ground, was not only welcomed news, it allowed the condition to remain officially invisible so as never to materialize as a health priority. This went on for nearly three decades until patients began to organize” (Fullwiley xxii).
“…sickle cell specialists’ biogenetic rendering of patients’ health overlooked how economic scarcity forced people to actually create unofficial economies of health care where their bodies would become sites to manipulate thresholds of pain and to condition decreased needs for painkillers and other low-tech but still costly treatments, on the one hand, and to dissolve the bounds of subjectivity and of pain beyond themselves to be shared, managed, and lived intersubjectively, on the other” (Fulwiley xxii-xxiii).
“What I hope to demonstrate in this book is the necessity of following emergent sickle cell health in its many biological, political, and cultural directions. Medical anthropologists must explore an inclusive mix of life and be as broad as possible in our analyses of genetic renditions of biological difference, as well as how such differences come to live within the scientific literature through specific grammars, such as association studies” (Fullwiley xxiii).
“Doing this allows us to see, in this case, how African states, postcolonial health care governance, cultural practices, and disease politics populate the family trees of the exceptional data points that—as DNA markers—are too often saddled with the task of explaining human biological difference alone” (Fullwiley xxiii).
Chapter 2: “Healthy Sicklers with ‘Mild’ Disease: Local Illness Affects and Population-Level Effects” (pp. 45-76)
“As discussed in the last chapter, clinicians and geneticists in Francophone sickle cell circles have adopted an optic of seeing African sicklers in terms of population groups that exhibit differences in disease expression. However, a key slippage occurs when scientists observe biological ‘outcomes’ and assume, as a first response, that these should be attributed to distinct genetic sequences, which those same populations possess at different frequencies. This chapter examines how such scientific methods and assumptions may miss complex congeries of behaviors and relationships that influence people’s disease experiences and biological expressions of sickle cell anemia” (Fullwiley 45).
“By engaging cultural frameworks of relations, notably of kin ties and social safety nets that mitigate sickle cell suffering for many, I hope to enlarge the conceptual terrain of how we view causal factors for varied disease manifestations” (Fullwiley 45).
“By analyzing local Senegalese discursive practices that name their sickle cell ‘mild,’ I bring affects —which extend beyond emotions to patients’ shared sentiments and the family ties that inspire health—into this picture. Put simply, people’s moral concerns of caring for the other, of going to incredible lengths to make family and loved ones live in health, is the human, intersubjective substrate that undergirds an experience of alleviated sickle cell stress, both bodily and socially, in Dakar today” (Fullwiley 45).
“Phenomenologically speaking, a ‘reality’ of sickle cell mildness in Dakar is the biosocial framework of relations with which health appearances tally. This is to say, reality is not a truth to be excavated, if only the social analyst could dig deep enough. Rather, it is made through care practices, political contingency, and social engagements where human actions contribute to and partially determine life possibilities” (Fullwiley 46).
“The bonds that people in Dakar form through this disease include putting an accent on the shared propensity of their blood to sickle, their commonly experienced pain that sickling brings on, and the widely referenced economic constraints that force people to train their bodies and their households to focus on relative health. In their efforts to manage both sickle cell crises and a larger structural crisis in their country’s health infrastructure that limits optimal biomedical care, people forge therapeutic economies where they circulate and share both pain and well-being” (Fullwiley 46).
“Although the sick take notice of and find comfort in the doctor’s touch, comment on the feelings of goodwill they sense from mindful providers, and, in some cases, pronounce a ‘family tie’ with the person overseeing their health or that of their child, it is outside of the clinic where they find significant therapeutic gains. These are in social supports and structures of family-based collective actions where people work to change the experiences of those suffering with sickle cell for the better” (Fullwiley 46).
“Increasingly within their organized patient network, Senegalese sicklers have begun to create groupings and even romantic ‘couplings,’ that many know are not ‘recommended,’ but that they stress have provided them with a culture of ‘confidants’ and ‘loved ones who can really understand them’” (Fullwiley 47).
“As of 2010, within the patient advocacy group in question, there are at least a half a dozen couples that claim to extract therapeutic value from their supports of romantic love, as well as from the larger advocacy network. In so doing they normalize their life prospects by entertaining marriage and the possibility of a future family. Through their affective ties they also succeed in enacting their biology as ‘milder’ than it would be without these biosocial links” (Fullwiley 47).
“People with sickle cell are actively trying to figure out how to deal with a mode of state management that threatens to compromise their hopes of simply being with their disease, as well as living with, dating, marrying, and mutually supporting others who are also affected. As will become clear, living with sickle cell in the Senegalese nation-state is defined by a biopolitics where these internal dilemmas and questions about how to go forward define people’s aspirations for normalcy” (Fullwiley 48).
“I show the ease with which people wield the materiality of ‘shared blood,’ while reviewing anthropological reflections on kinship and the social life of informal economies in Africa. This background will provide the framework to see how mild sickle cell anemia becomes biosocially structured through political-economic contingency and networks of informal therapeutic economies in Dakar in the absence of state resources” (Fullwiley 48).
“Such biosocial relations of caring, in different configurations, allowed people to find a certain naturalness of affinity through kin idioms that whittled down clear distinctions between subject and object, personal ‘ownership’ of suffering and disease, and self as separate from the other in pain” (Fullwiley 49).
“Kinship understandings and varied forms of biosocial affinities are a crucial source of both physical and cultural practices of survival in Senegal more broadly. It is through such relations that sicklers in Dakar are able to reduce their disease burden, in some cases, and experience their sickle cell status as a kind of existential normalcy, in others” (Fullwiley 49).
“Sicklers, their families, and newly created disease advocacy networks of persons ‘attached’ as kin absorb, emotionally redistribute, and in some cases, deflect sicklers’ pain and suffering. These networks of support, of both literal and metaphorical kith and kin, provide subtle and direct sources of alleviation and improved health” (Fullwiley 50).
“Sociosomatically, those affected distribute and share the intensity of their genetic disease with others. Through openness and a willingness to take on each other’s pains, many have succeeded in mitigating the severity of suffering alone. Here it is the constitutive order of kinship, economy, and biology that allows individuals a leg up in their struggle for personal and family health in a context where they experience daily that the formal economy and the state health system work against them” (Fullwiley 51).
“This investment in the sick family member, patient, or comrade who shares the political struggle to organize in the form of disease advocacy often reoriented people’s own visions of ‘normal’ norms that were rooted in explicit Senegalese customs that emphasize the necessity of marriage and biological reproduction. As some people overtly questioned and then reworked social norms of marriage, they suspended or sublimated others, notably with regard to reproduction” (Fullwiley 51).
“Economic supportive ties do not always co-constitute kinship and lived biology, however. Yet, when they do, we can begin to see how the work that the bond, or chain, of kinship achieves, as a form of relatedness that is not at all confined to birth-family blood links” (Fullwiley 51-52).
“Taken as an aggregate, with many individuals hustling to attain the goods to secure survival, Senegalese sicklers ameliorate their prescribed fates, partake in rendering their disease ‘mild,’ and often attain adulthood despite a staggering lack of medical technology and standard interventions and resources that constitute sickle cell care in the United States and France” (Fullwiley 52).
“In pointing out the failures of global logics to incorporate impoverished nations into more equitable market relations—through structural adjustment programs, as well as more palatable programs to empower those in poverty through microfinance or decentralization made possible by the upsurge of NGOs—this recent economic anthropology highlights the role of informal actors that sustain state coffers and civil institutions” (Fullwiley 52-53).
“What we see in Senegal during this period is the inception of a pattern that was later repeated in many African countries that underwent structural adjustment: declines in wages and wage employment in the formal sector not only resulted in job losses for countless individuals but also severely compromised governments’ ability to provide health education and welfare services broadly (Turshen 1999, 60–61)” (Fullwiley 55).
“People often contemplated how difficult it was for them to sustain the chronic cost of keeping their children with sickle cell ‘crisis- free’ and alive, yet they also offered expansive conceptions of kin-inspired safety nets that blended economic and social supports, a pattern perpetuated in the establishment of the sickle cell care network, the ASD. Their predicaments made me realize that despite the many recent optimistic reports on Senegal’s economic growth, from those published by the World Bank, to profiles generated by the World Health Organization, increased income means little when life—and maintaining it—simply costs more than it did in the past, and when the state shouldered what are now withering social securities” (Fullwiley 56).
“…the heightened demands that people ‘participate’ in securing their own health have made many switch from relying on currencies of money to investing in improvised currencies of care that might partially absorb their disease pain and life difficulties” (Fullwiley 56-57).
“Now I turn to people’s specific stories that illustrate how economic, affective, and material exchanges that inflect social bonds, and vice versa, absorb disease pain. As we will see, people manage the scarce resources they have, while trying to create a stock of care remedies, which draw on varied practices, including manipulations of bodily thresholds, gifting therapeutic goods, and undertaking subjective ‘training’ dictated by household cash flows and constraints in this wider context of prolonged economic uncertainty” (Fulwiley 57).
“For many, economy must be thought of more broadly than purchasing power and available health care goods. Home economics—such as a father’s calculated investments in a sick daughter’s well-being—and the human attachments to therapies circulated in society, such as discounted vaccinations offered by a friend, or fagara purchased by a sympathetic onlooker, also make it clear that the sociability of goods and shared sentiments sustain relationships and establish interdependence through networks of investment and debt-gifting” (Fullwiley 57).
Rokhoya Sylla: “It was in part because of a profound realization that she was ‘not alone in this disease’ that she began to express her feelings more openly. Her disease had been ‘mild’ but at what cost? The normalization of her illness was rooted within the love of her caring family, yet it was also situated within a context of broader economic precariousness, which she observed all around her. Most recently, she had suffered from survivor’s guilt as she witnessed a neighbor with less educated and capable parents die from the same disease because, in her words, ‘he lacked my health.’ She also understood that her near-total health was rare, and she simply credited her father’s care. Nonetheless, by gauging the worst cases of the disease around her and comparing them with her own, she imagined that her livelihood was due to a very thin buffer, family care, which separated her suffering from that of others. Rokhoya suffered nonetheless; she lived emotionally bewildered at the thoughts of her special status, her family’s sacrifice, and the biosocial inequality that somehow cast the die in her favor” (Fullwiley 61-62).
“In the group, she found a family of shared blood whose proclivity to, and semi-normalization of, silent suffering mirrored her own—except for the fact that their organization was now giving a voice to the void” (Fullwiley 63).
“Similarly, in Senegal, when economic privation characterizes the life worlds of those with chronic disease, people normalize illness as an aspect of the everyday. In part, it is this patterning that renders Magueye’s [Magueye Ndiaye] disease ‘mild’” (Fullwiley 67).
“Senegalese family pressures to reproduce, the physician’s lectures against knowingly bearing children who might have the disease, and even the mission statement of the ASD in its ‘fight against sickle cell’ have laid out certain norms of conduct that collided with Magueye’s hope to pursue his relationship with Safietou” (Fullwiley 72).
“In Senegal, as elsewhere, biological kinship remains an impressive force that continues to shape people’s options for the future” (Fullwiley 76).
“In conversations with other sicklers I met in Senegal, the domain of marriage is where the level of health and the new norms sicklers acquire through informal care strategies collide with the limits imposed by the genetic rules and societal taboos related to passing on their disorder” (Fullwiley 76).
—
Note: The featured image for this post is Figure 1.1 (Fullwiley, p. 16), a sickle cell haplotype map.